UMN Lesions:
1) Cortex=cortical signs(VAAN) visual field defects, altered mental status, aphasia, neglect
2) Subcortical=dense hemiplegia with no cortical signs
3) Brainstem=crossed paralysis
4) Spinal Cord=sensory level with bladder involvement
LMN Lesions:
5) Anterior Horn Cells=no sensory impairment with mixed UMN & LMN signs
6) Nerve Roots=pattern of loss follows a specific dermatomal/myotomal distribution
7) Plexus (brachial and lumbosacral)
8) Peripheral Nerves=glove& stocking plus areflexia
9) Neuromuscular Junction-fatigability (do a H-test to look for exertional diplopia)
10) Muscles=myopathic facies
Most common sites of intracranial hypertensive bleed:
1) Basal Ganglia
2) Thalamus
3) Brainstem(Pons)
4) Cerebellum
Gaze Preference in Stroke
Example: Patient with Right cortical infarct shows tendency to look
at the right side
Lesion is at Frontal Eye Field (FEF)
Post Stroke Seizure
seen in patients with cortical stroke, usually in day 3-5 post stroke.
(cortex is where the generation of impulse starts!)
Testing Neglect (cortical signs in non-dominant hemisphere)
Sensory, Visuo-, Spatial-
1) Sensory neglect- refer video (coming out soon!)
2) Visuo- must firstly establish that patient has no visual field defect
3) Spatial- either clock drawing or the line bisection test.
Types of Dysphasia (cortical signs in dominant hemisphere)
1) Receptive (wernicke's)
2) Expressive (broca's)
3) Repetition defect (arcuate fasciculus)
4) Nominal (??)
Types of lacunar stroke (lesion less than 15mm on CT)
(Lipohyalinosis and Microatheroma)
1) Pure motor
2) Pure sensory
3) Mixed motor & sensory (sensorimotor)
4) ataxic hemiplegia
5) clumsy-hand dysarthria
Ischaemic Penumbra(on non contrast CT):
Salvageable brain tissues around an already ischaemic area
Guillain-Barre Syndrome types:
1) Acute Inflammatory Demyelinating Polyradiculoneuropathy(AIDP)
-pathology is due to demyelination
-Nerve Conduction Studies(NCS) can diagnose other subtypes:
2) AMAN - Acute Motor Axonal Neuropathy
3) AMSAN - Acute Motor-Sensory Axonal Neuropathy
-pathology is due to axonal damage instead
and
4) Miller-Fisher Syndrome(triad of ataxia, ophthalmoplegia, areflexia)
Long Tract Signs = Corticospinal Tract (UMN lesion)
Generalise Areflexia + Glove & stockings distribution = Peripheral neuropathy
Causes of Predominantly Motor peripheral Neuropathy:
1) AIDP
2) CIDP
3) Lead poisoning
4) Porphyria
5) Charcot-Marie Tooth
Romberg's Test = to rule out sensory ataxia!
Pseudoathetosis = failure of joint position sense/sensory ataxia
Internuclear Opthalmoplegia(INO)
causes: Multiple Sclerosis, Brainstem Stroke
*Lesion at the ipsilateral Medial Longitudinal Fasciculus(MLF)
For example, a patient with right sided MLF lesion, during an attempt
to perform a left gaze, there will be: 1) failure of adduction in the right eye
and 2) nystagmus in the left eye.
Imagining this as the right eye is slower(can't adduct), and the left eye will be
like, come on, catch me up(thus nystagmus).
Phenytoin can induce Cerebellar Atrophy
In Idiopathic Parkinson's Disease, one side is usually more severe
than the other.
With intact facial nerve, the complete closure of the eyes shall
hide the eyelashes completely as well
POEMS syndrome
Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal Protein, Skin Changes
Carvenous Sinus
Cerebellopontine Angle
Causes of young stroke(CTAV)
Cardioembolic (bubble echo TRO patent foramen ovale causing paradoxical stroke)
Thromboembolism(hypercoagulable states)
Autoimmune Conditions
Vaculitis, VDRL
examples: antiphopholipid syndromes, hyperleukocytosis, polycythemia, cerebral lupus,
CADASIL, MELAS, neurosyphilis
In large vessel ischaemic stroke, treat hypertension only when BP exceeds 220/120 mm Hg
using IV labetalol +/- oral antihypertensives
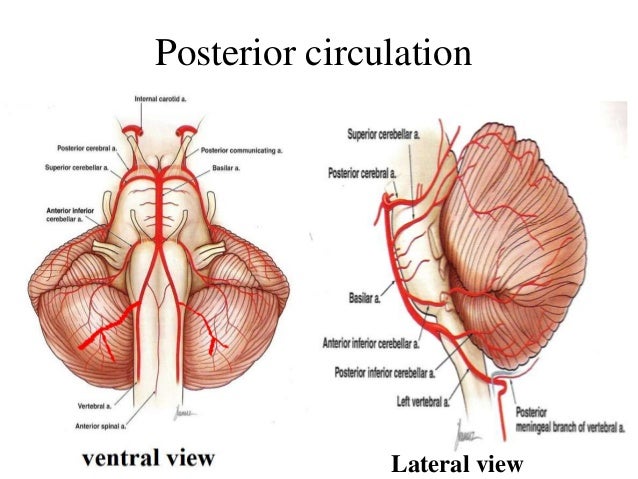
Symptoms to ask in Brainstem lesions:
1) Double Vision (3,4,6)
2) Facial Numbness (5)
3) Facial Asymmetry (7)
4) Hearing Loss and Vertigo (8)
5) Swallowing difficulty (9,10)
6) Dysarthria (12 due to spastic tongue)
Gallery:
*From google image unless stated otherwise



xxxxxxx


No comments:
Post a Comment